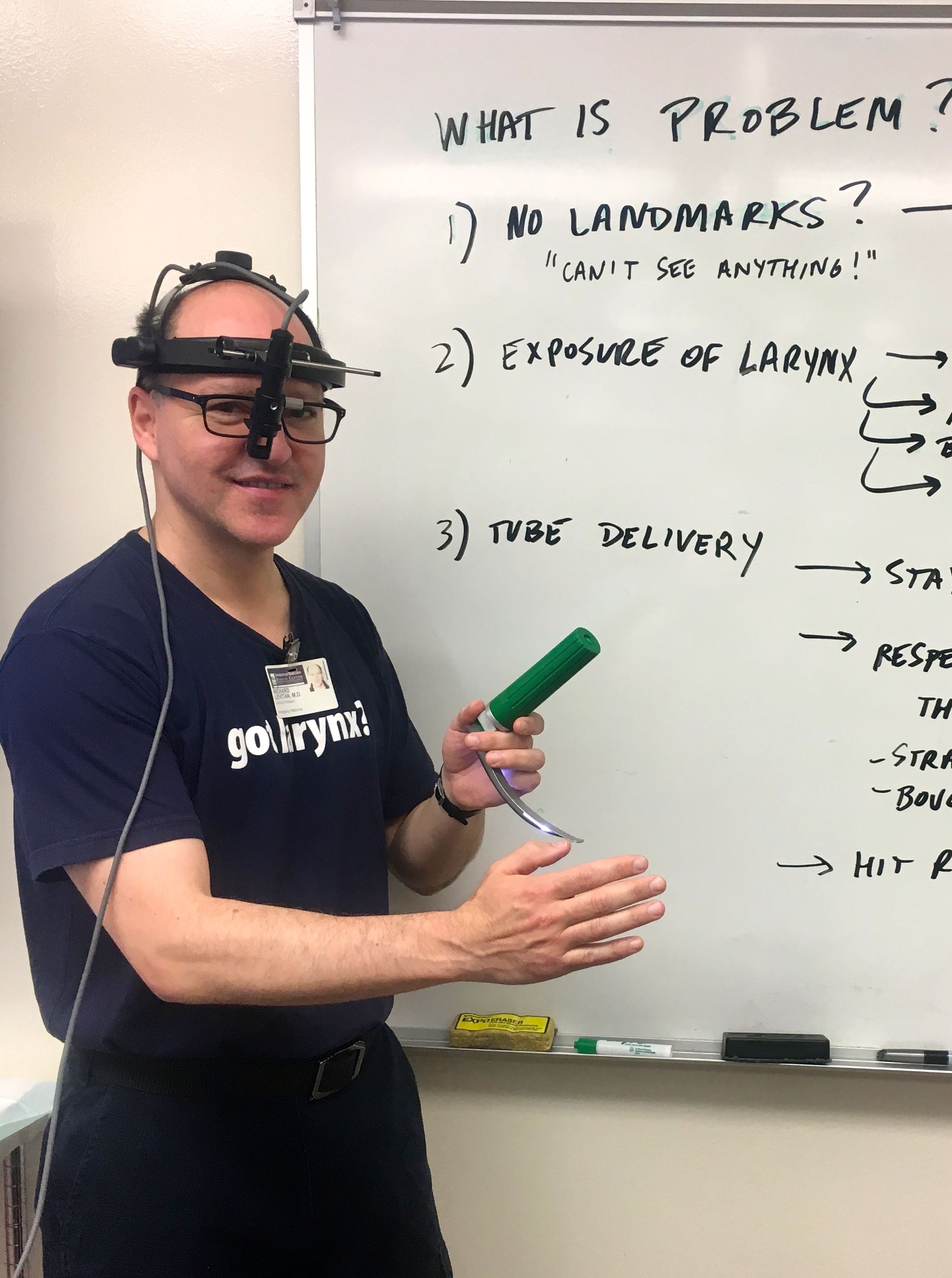
Dr. Richard Levitan
Dr. Levitan was in the first class of Emergency Medicine residents at Bellevue Hospital (1990-1994), and subsequently worked in academic, high-volume, inner-city trauma hospitals in NYC and Philadelphia for 25 years (Bellevue, Lincoln, Penn, Einstein, Jefferson). Starting in 2012 he began working in rural, critical care access hospitals. He now balances this clinical activity with teaching courses, speaking engagements, and device development.
In addition to the Airway Cam (1994), his inventions include the Levitan FPS optical stylet (Clarus Medical), the Control Cric (Pulmodyne Inc.), and the Universal Stylet Bougie (USB, Intersurgical Ltd.). He has been involved in numerous device development projects with various manufacturers. He did early design testing and wrote the first published paper on the I-gel supraglottic airway.
Dr. Levitan has designed and built his own unique intubation manikins (with anatomic variation) for teaching laryngoscopy (the Airway Training Series), as well as a unique anatomically correct surgical model (CRICALOT), which uses an inexpensive three-layer skin analogue.
He has published extensively on laryngoscopy and airway management. Now working in rural critical access hospitals, he used to hold appointments at the Hospital at the University of Pennsylvania, Jefferson Medical College, Dartmouth (Geisel) School of Medicine, as well as a Visiting Professor appointment at the University of Maryland School of Medicine.
The Airway Cam Direct Laryngoscopy Video System
The Airway Cam imaging system was invented by Dr. Levitan in 1994 when he was an emergency medicine resident at Bellevue Hospital in NYC. Recognizing the challenges of skill acquisition and the lack of imaging, he developed a means of displaying direct laryngoscopy as seen by the operator. The Airway Cam is a head mounted video camera, optically aligned with the dominant pupil, that is able to image direct laryngoscopy from start to finish; it was patented in 1998. He invented a grading system for laryngeal exposure with imaging called the Percentage of Glottic Opening Score (POGO score), which has been used my researchers worldwide. The Airway Cam and POGO scoring has been used by Dr. Levitan in numerous research papers on laryngoscopy, including head-elevated laryngoscopy positioning (HELP), bimanual laryngoscopy, and comparisons of cricoid pressure, BURP, and bimanual laryngoscopy.
Cadaveric Research and Training.
—Airway Cam Educational Materials
Dr. Levitan has been involved with airway education and research since 1994, using the Airway Cam to record procedures in live patients and cadavers. He started cadaver-based airway management courses beginning in 2001 with Dr. William J. Levin. Four more than two decades the course was run with Dr. Kenneth Butler (University of Maryland), James T. Pisaturo EMT-P, and Dr. Jorge Cabrera (Jackson Memorial Hospital), until 2022. The success of the Baltimore course has led to Dr. Levitan’s involvement with cadaver courses now offered annually in Australia, and sporadically in the UK, and New Zealand. CLICK HERE FOR AUSTRALIA CADAVERIC COURSES.
Following the pandemic, the course has now resumed in Texas at the Centre for Emergency Health Sciences, in Bulverde. Dr. Levitan teaches these classes with Dr. Salim Rezaie (REBEL EM). CLICK HERE FOR TEXAS CADAVERIC COURSES.
Research we have conducted in cadavers has defined a best practice approach to laryngoscopy and surgical airways (now widely adopted) that we created and promoted including: ear-to-sternal notch positioning, epiglottoscopy, bimanual laryngoscopy, straight-to-cuff stylet shaping, the laryngeal handshake, and other techniques.
Airway Cam educational materials–videos, book, and pocket guides–have been critically acclaimed by leading medical journals around the world.
Improving Cricothyrotomy
—The Laryngeal Handshake, Sternal Stabilization & The Cartilaginous Cage
Surgical cricothyrotomy is a rarely necessary but critical airway procedure that emergency providers must know how to perform. Teaching this procedure has always been a part of the Baltimore course. Through thousands of participants and decades of cadaveric courses, Dr. Levitan developed a means of localizing the thyroid cartilage (and adjacent hyoid and cricoid cartilages) called the “laryngeal handshake.” Traditional instruction teaches that the first step of a surgical airway is localizing the cricothyroid membrane, but it is a fine motor skill dependent on feedback dependent on 1 square centimeter of the index finger. It is particularly difficult in obesity, and much less evident in woman than in men. Realizing that the first skin incision should be a vertical incision (allowing wound exploration and verification of the cricotyhroid membrane), Dr. Levitan developed the “laryngeal handshake.” This is a coarse motor skill to assist operators in recognizing the laryngeal cartilages and midline. The hyoid, thryoid and cricoid cartilages make up a rhomboid that can easily moved from side to side. The most reliable landmark in the surgical airway is the broad lamina of the thyroid cartilage (and this is reliably palpable, even in women). “Sternal stabilization” involves stabilizing the dominant hand on the sternal while making both the initial vertical skin incision, and the subsequent horizontal cricothyroid membrane incision. The “cartilaginous cage” is a descriptive term for teaching the anatomy about the larynx, highlighting the “cage” of cartilage surrounding the cricothyroid membrane (the thyroid lamina above, the anterior cricoid ring below, and the inferior cornu of the thyroid cartilage, overlapping the cricoid cartilage laterally on either side). The final component of this “cage” is the high and rigid back wall of the cricoid cartilage.
In the 2015 the Difficult Airway Society incorporated the laryngeal handshake into their guidelines from front of neck airway access: https://academic.oup.com/bja/article/115/6/827/241440
Researching the optical and mechanical challenges of tracheal tube delivery.
Studying stylets, bougies, and hyperangulated stylets—and development of the USB.
Twenty five plus years of regular cadaver labs has given Dr. Levitan the opportunity for intensive investigation into the optical and mechanical challenges of inserting tracheal tubes into the trachea.
Tracheal tubes interact with the corrugation of the rings and the inclination of the trachea as it descends into the thorax. Curvilinear tubes can block the line of sight to the target (with both direct and video laryngoscopes), and though video laryngoscopes often make exposure much easier, hyperangulated blades may make tube delivery more difficult.
Stylets allow molding the tracheal tube into a straight-to-cuff shape that improves the optical challenges of tube delivery by staying out of the line of sight. Bougies have a smaller outer diameter than stylets and are less likely to block the line of sight during direct and video laryngoscopy. Hyperangulated rigid stylets are used with hyperangulated blades to direct tubes around the tongue, but their rigidity and dimensions prevent them from being fully inserted into the trachea.
The Universal Stylet Bougie (USB) is a novel universal introducer developed over ten years of prototype testing by Dr. Levitan. It is a universal stylet and bougie (hence the acronym “USB”)—for conventional Macintosh and hyperangulated blades, whether using direct or video laryngoscopy. It is a better bougie than a standard bougie, and a better stylet than a standard stylet. It can be used a bougie in standard fashion, or with a hyperangulated shape (for hyperangulated video laryngoscopy). The USB can also be used as a stylet in either standard straight-to-cuff shape, or as a hyperangulated stylet. It has a number of novel design features: a hexagonal cross-sectional shape, and a pre-molded overall size (overall package dimension is the same as a tracheal tube). Perhaps the device’s most remarkable feature is it’s mechanical amplification of tracheal rings—making confirmation of placement in the trachea nearly universal. See below for more information on the USB, or contact Intersurgical Ltd. to learn more.
O’s Up the Nose!
—NO DESAT: Nasal Oxygen During Efforts Securing A Tube.
—Revolutionizing intubation worldwide.
Intubation, especially using RSI medications, was frequently complicated by peri-procedural desaturation. Apart from pre-oxygenation, there were no techniques employed to prevent destauration during laryngoscopy and intubation.
Upon hearing of low flow oxygen to extend safe apnea in the morbidly obese in elective anesthesia (2011), Dr. Levitan started experimenting with higher flows (albeit through standard nasal cannulas) in emergency RSI situations. NO DESAT (Nasal Oxygenation During Efforts Securing A Tube) went viral after Dr. Levitan collaborated with Dr. Scott Weingart. Disseminated through FOAM ED (emcrit and other podcasts), and a seminal 2012 paper in Annals of Emergency Medicine, this technique has gained worldwide acceptance in emergency medicine, critical care, and anesthesia.
In the 7 years since it’s original introduction, critical appraisals, and meta-analyses of apneic oxygenation have validated it’s utility across many settings (PubMed link on apneic oxygenation AND intubation).
OOPS—Oxygen On Pull the mandible forward, Sit the patient up—using standard nasal cannulas at high flows to rapidly reverse desaturation in procedural sedation–has been promoted by Dr. Levitan as a better initial response to hypoxia than bag mask ventilation.
Setting the standard for positioning: The Ear-to-sternal notch line
Positioning is critical for for both the mechanics of laryngoscopy and also the physiology of oxygenation. With the goal of defining the ideal position for intubation and airway management, Dr. Levitan created an objectively defined end point—-the ear-to-sternal notch line.
Ear-to-sternal notch line is a horizontal line from the external auditory meatus to the sternal notch. This raises the head relative to the chest; the face place should be horizontal to the ceiling. This ideal positioning applies to both adults and children.
The ear-to-sternal notch line has been widely adopted across multiple disciplines. It has been validated with MRI anatomic studies by Dr. Keith Greenland. It has become the worldwide standard for intubating the morbidly obese, after a landmark laryngoscopy study by Drs. Brodsky and Collins (Stanford) in which Dr. Levitan collaborated.
USB - Universal Stylet Bougie
In 1949 Robert Macintosh promoted the use of a gum elastic catheter to aid intubation. The USB is the first clinically significant redesign of this useful airway adjunct. It has many novel features enhancing performance and handling including: a hexagonal cross sectional shape, a pre-molded small shape that can be unbent as needed, enhanced detection of the tracheal rings, use a regular bougie, a hyperangulated bougie, a regular stylet and a hyperangulated stylet.
The Control Cric - A Surgical Cricothyrotomy Device Designed for the Military, Now Available to All
Unique bi-directional cutting blade, a hook/plcae holder that is embedded in the wide grip handle, and a short curvilinear introducer that allows easy detection of the tracheal rings—without visualization, light, listening with a stethoscope, or fine motor skills. Silicone strap secures the non-kinkable airway tube in any environment—even in the sand, water, or snow.